Updated November 3, 2025
Proper coding and a clear understanding of remote patient monitoring (RPM) billing requirements are essential as RPM continues to grow. With increased scrutiny from regulators, including upcoming audits by the Office of Inspector General (OIG), practices must ensure they are billing CPT 99453 and other RPM codes correctly. Accurate coding not only protects against audits and claim denials but also ensures providers receive full reimbursement for the care they deliver. As RPM adoption expands, staying compliant with billing guidelines is crucial for maintaining a successful and sustainable program.
What is CPT Code 99453?
CPT 99453 is a medical billing code used for RPM services. Specifically, it covers the initial setup and patient education for remote monitoring devices. This includes training patients on how to use the device and ensuring they can transmit data effectively to healthcare providers.
Key Details of CPT Code 99453
- Purpose: Covers the setup and onboarding of a remote physiologic monitoring device
- Reimbursement (2026): $21.71 (National Medicare non-facility rate)
- Billing Limitations: One-time billing per patient per episode of care
Who Can Bill for CPT 99453?
Only a qualified healthcare professional, like a physician, nurse practitioner, or physician assistant, who is eligible to bill for evaluation and management (E/M) services can bill for CPT code 99453
This code can be billed by eligible healthcare providers, including:
- Physicians
- Advanced practice registered nurses (APRNs)
- Clinical staff under general supervision of a physician or qualified health professional (QHP)
Billing Requirements
- The device must meet the FDA's definition of a medical device.
- The patient must be consented in a RPM program.
- Only one provider can bill for 99453 once per patient per episode of care.
- CPT 99453 can be billed in conjunction with other RPM codes (e.g., 99454, 99457) but only once per device setup.
When Can CPT Code 99453 Be Billed?
CPT 99453 can be billed only once per patient per monitoring program initiation, regardless of the number of devices set up. The provider can bill once after completing device setup and patient training.
- If a patient receives multiple RPM devices (e.g., a blood pressure monitor and weight scale), only one billing instance is allowed.
- CPT 99453 is to be billed in the first month the patient delivers 16 days worth of device readings (i.e. meets billing criteria for CPT 99454)
- Rebilling for CPT 99453 is not permitted unless the patient undergoes a new episode of care that requires new device setup and training.
What Devices Qualify for CPT 99453?
As RPM has gained popularity, the number of available RPM devices has also increased. However, not all devices that capture patient data qualify for RPM billing. To be reimbursable under CPT 99453, a device must meet specific criteria, including compliance with FDA regulations and the ability to transmit data wirelessly in real time. Federal guidelines require that "physiologic data must be electronically collected and automatically uploaded to a secure location where the data can be available for analysis and interpretation by the billing practitioner." This ensures that RPM devices provide clinically useful insights while maintaining regulatory compliance.
Here are some common RPM devices that qualify under CPT 99453:
- Blood pressure monitors — Used for monitoring hypertension and cardiovascular health, helping providers assess trends and adjust treatment plans accordingly.
- Weight scales — Often used for managing conditions like congestive heart failure (CHF) and obesity, allowing clinicians to track fluid retention and weight fluctuations.
- Pulse oximeters — Measure oxygen saturation (SpO2) levels and are crucial for managing patients with chronic respiratory diseases, post-COVID monitoring, and conditions like COPD.
- Blood glucose monitors — Essential for diabetes management, these devices help patients and providers track blood sugar levels in real time, leading to better glycemic control.
When selecting RPM devices, healthcare providers must ensure that the devices they use meet the FDA's definition of a medical device. An eligible RPM device may require 510(k) clearance, pre-market approval, or a waiver. Additionally, devices must support automatic and secure data transmission to facilitate remote monitoring and provider decision-making. Choosing legitimate, RPM devices not only ensures proper reimbursement but also enhances patient care by delivering reliable, real-time health insights.
CPT 99453 vs. Other RPM Codes
CPT code 99453 covers the initial setup and patient education for RPM, ensuring that patients understand how to use their devices effectively. Proper documentation and billing for this code are essential for compliance and reimbursement.
|
CPT Code |
Description |
Avg. Reimbursement (2026)* |
Billing Frequency |
|
99453 |
Device setup & patient education |
$21.71 |
One-time |
|
Monthly supply & data transmission (16+ days) |
$47.43 |
Once in a 30-day period |
|
|
Monthly supply & data transmission (2–15 days) |
$47.43 |
Once in a 30-day period |
|
|
Initial 10-20 minutes of care management time |
$26.05 |
Once, Monthly |
|
|
First 20 minutes of RPM management |
$51.77 |
Once, Monthly |
|
|
Each additional 20 minutes |
$41.42 |
Monthly |
*Estimated reimbursement values as of November 2025
However, 99453 is just one of several CPT codes used in RPM billing. Here is a quick look at the six most common RPM CPT codes. Note: For a comprehensive overview of all RPM CPT codes and their specific applications, check out our guide here.
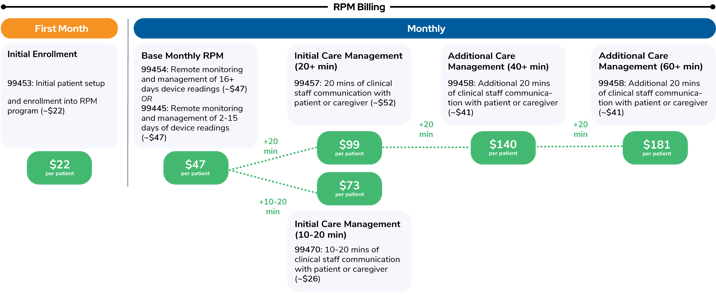
RPM billing follows a structured process based on time spent managing a patient's care. A practice typically provides around 20 minutes of RPM care management each month, leading to an estimated monthly reimbursement of approximately $94 per Medicare beneficiary. However, with additional monitoring and services, reimbursement can increase, with a maximum potential of around $183 of Medicare reimbursement per patient per month. Understanding how these billing components work together can help practices optimize their RPM programs while ensuring compliance and appropriate reimbursement.
Here's what RPM billing looks like in 2026 (with the addition of RPM CPT codes 99445 and 99470):
Best Practices for Billing CPT 99453
To ensure smooth, appropriate reimbursement, follow these best practices:
- Confirm patient eligibility under Medicare or private payers
- Document the training session, including date, time, and content covered
- Ensure devices meet FDA medical device requirements
- Bill only once per patient per care episode
- Use proper coding combinations (e.g., pair 99453 with CPT 99454 for ongoing monitoring)
CPT 99453: The RPM Setup and Patient Education Code
CPT code 99453 is an essential component of remote patient monitoring billing, covering the initial setup and patient education. To ensure compliance and complete collections, healthcare providers should adhere to CMS guidelines, properly document patient training, and use qualified RPM devices.
By implementing CPT 99453 effectively, providers can enhance patient engagement, improve health outcomes, and increase practice revenue through RPM services.
Get Started With RPM Today!
Learn how to bill 99453 and other RPM codes correctly while ensuring compliance and increased reimbursement. Schedule a demo with our care management experts to see how our platform simplifies RPM and helps you achieve improved patient outcomes.
CPT Copyright 2025 American Medical Association. All rights reserved.
CPT® is a registered trademark of the American Medical Association.
Disclaimer
Health economic and reimbursement information provided by Prevounce is gathered from third-party sources and is subject to change without notice as a result of complex and frequently changing laws, regulations, rules, and policies. This information is presented for illustrative purposes only and does not constitute reimbursement or legal advice.
Prevounce encourages providers to submit accurate and appropriate claims for services. It is always the provider’s responsibility to determine medical necessity, the proper site for delivery of any services, and to submit appropriate codes, charges, and modifiers for services rendered. It is also always the provider’s responsibility to understand and comply with Medicare national coverage determinations (NCD), Medicare local coverage determinations (LCD), and any other coverage requirements established by relevant payers which can be updated frequently.
Prevounce recommends that you consult with your payers, reimbursement specialists, and/or legal counsel regarding coding, coverage, and reimbursement matters.
Payer policies will vary and should be verified prior to treatment for limitations on diagnosis, coding, or site of service requirements.
.png)
