Last updated October 2024
One of the more substantial, recent developments in the way healthcare is delivered in the United States concerns remote patient monitoring (RPM), also referred to as remote physiologic monitoring. RPM has technically been around since the early 1970s (with its roots dating back to the 19th century!), but it's been thrown into the spotlight over the past few years thanks to the pandemic and is now experiencing rapid adoption. That comes as no surprise considering the significant and wide-spread benefits of remote patient monitoring.
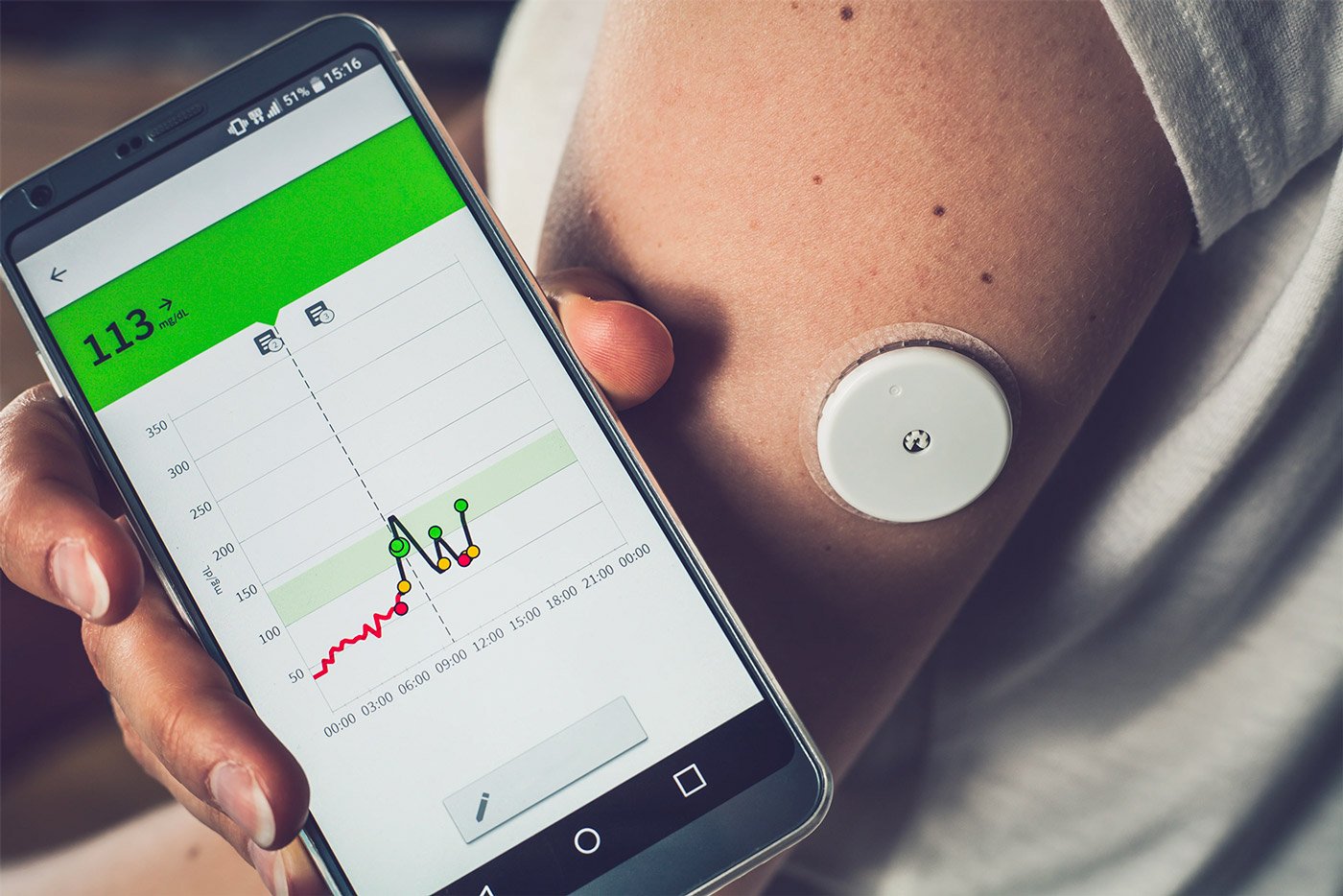
In a nutshell, remote patient monitoring is a way for a care provider to closely monitor a patient's chronic health conditions without requiring the patient to physically visit a healthcare organization. To deliver RPM, practitioners choose one or more devices that their qualifying patients can use outside of the facility to collect health data and then transmit that data securely back to the organization for evaluation.
There are many different RPM devices on the market, each with its own purpose in tracking symptoms of a specific chronic disease. For example, blood pressure cuffs, as the name suggests, track and report blood pressure and heart rate information from patients with hypertension and heart disease while a blood glucose monitor (i.e., glucometer) tracks and reports blood sugar information for diabetics. Other available devices include weight scales, which can be useful in tracking water retention in patients with heart disease, and spirometers to measure lung function in patients with asthma and chronic obstructive pulmonary disease (COPD). Patients are instructed on how to use their specific device and then the data is collected and transmitted over a secure Bluetooth or cellular connection to a user-friendly application like Prevounce, which is then accessed by the provider organization.
Expanding Usage of Remote Patient Monitoring
There are several factors contributing to the upward trend of remote patient monitoring usage. Between elevated public health concerns associated with the pandemic and challenges associated with delivering care to an aging population, RPM looks like it's here to stay. Practitioners across the country are finding this virtual service to increasingly valuable as it is a safe and effective means of maintaining the delivery of healthcare to some of their most vulnerable patients.
For example, a recent study published in the Journal of the American Heart Association demonstrated that a remote clinical management program delivered significant improvements in blood pressure control and increased home blood pressure monitoring. The American Heart Association cites additional research demonstrating that remote cardiac monitoring can greatly reduce patient blood pressure compared to typical care and self-monitoring alone. As another example, studies of remote pulmonology monitoring have revealed that such interventions are specifically associated with improvement in asthma control and decrease in rescue medication use, among other benefits.
Another appealing quality of RPM is that the service is covered by a growing list of insurers and reimburses well, as we will discuss further below.
One other noteworthy factor driving the increase in remote patient monitoring usage is that the United States is facing a shortage of healthcare providers. The Association of American Medical Colleges (AAMC) projected a shortage of between 37,800 and 124,000 physicians by 2023, and a primary care practitioner shortage of as many as 48,000 practitioners in the same period.
Compounding the physician shortage is that the country is expecting an overall population growth of more than 10% with people over the age of 65 increasing by more than 42% over the same period. Since healthcare provider shortages are inevitable, remote patient monitoring represents a smart solution to maintaining quality patient care, expanding access to care, and reaching and supporting more patients efficiently and effectively.
The Real Cost of Chronic Health Conditions
Many Americans are under the impression that heart disease, obesity, diabetes, COPD, and other diseases and conditions are par for the course of aging and do not require ongoing attention. Yet many of these chronic diseases can be managed effectively to reduce the impact they have on quality of life. Unfortunately, our reactive way of trying to treat such chronic conditions when symptoms arise instead of managing them is costing American's a great deal of money. Currently, the United States spends roughly $4.9 trillion on treating chronic and mental health conditions, reports the Centers for Disease Control and Prevention (CDC). That's nearly 90% of our total annual healthcare expenditures.
The cost of healthcare is a painful pill to swallow for everyone. We are experiencing the expensive effects of chronic health conditions at alarming rates, but it doesn't look like we're going to get healthier any time soon either unless we make some meaningful changes. Consider the following about common chronic conditions that can be effectively managed by practitioners and patients by leveraging remote patient monitoring:
- Heart disease: One-third of all annual deaths in the United States are attributed to heart disease and stroke. That's more than 859,000 Americans. Equally concerning is the fact that these two diseases alone cost our healthcare system around $200 billion annually, and cost U.S. employers about $130 billion annually in lost productivity.
- Diabetes: The United States currently has more than 34 million people living with diabetes and another 88 million sitting on the proverbial diabetic cliff known as prediabetes. Alarmingly, diabetes is costing Americans more than $325 billion in medical and lost productivity costs.
- COPD/asthma: The current projected cost of chronic lung issues is around $50 billion annually, with the condition causing U.S. workers to miss collectively more than 16 million days of work per year.
Thanks to the benefits of remote patient monitoring, practitioners and patients are finding that managing these and other chronic conditions is often much easier than they believed was possible.
The Value of Remote Patient Monitoring for Patients
Let's take a closer look at five ways patients benefit from remote patient monitoring.
- Better access to the healthcare team. Since RPM devices report real-time health data, practitioners are kept in the loop on their patients' current health status, providing patients and caregivers with the ability to more quickly identify and respond to any concerning developments.
- Fewer trips to the office. This means fewer expenditures in both time and money for travel. For patients living in rural areas, who may need to travel long distances for specialty care, this reduction in travel requirements is significant for improving access and care.
- Improved quality of care. With RPM, practitioners gain a more holistic understanding of a patient's health condition, which can lead to more accurate adjustments in medications, fewer emergency room visits, and more time between in-office visits.
- More control over personal health. RPM typically comes with a user-friendly application for a phone or tablet that provides patients with instant analysis of their wellbeing. With this information, under the guidance of their care team, patients can make small adjustments to their daily lifestyle that can strengthen management of a condition and help them better recognize abnormal changes and developments.
- Better support and education. Since the healthcare team receives more detailed information about a patient's health status, practitioners can provide more personalized support, education, and engagement that can help ensure patients follow their treatment plans.
Financial Benefits of Remote Patient Monitoring
As noted, remote patient monitoring doesn't just deliver clinical and operational benefits. It provides financial benefits to patients and practices, which are worth exploring further.
Updates by the Centers for Medicare & Medicaid Services (CMS) to rules and reimbursement guidelines for remote patient monitoring over the past several years have helped the service see significant increases in adoption and expansion. Officially covered by original Medicare, CMS has outlined coverage rules that Medicare Advantage plans must also follow. Most other private insurance companies have followed the lead set forth by Medicare and increased their reimbursement.
For Medicare patients, they should expect copays until they meet their deductible. Once the deductible is met, remote patient monitoring is covered at 80% and beneficiaries can expect to pay on average about $25 per month for each month of monitoring. While this might seem significant, consider the real cost of in-person office visits for close monitoring of chronic health conditions. Between travel time and expenses, which can add up very quickly, $25 monthly seems like a small price to pay. Another consideration is the cost of hospital admission for unchecked exacerbations of chronic diseases, which in some cases can total in the several thousands.
Meanwhile, for organizations with remote patient monitoring programs, RPM remains a lucrative Medicare care management program — one whose value and financial benefits increase further when combined with the likes of chronic care management to create a comprehensive care management program. To learn more about RPM coding, billing, and reimbursement, check out this blog and download this billing guide.
Benefits of Remote Patient Monitoring for the U.S. Healthcare System
The benefits of remote patient monitoring for practitioners and patients are clear, so let's look at how RPM helps the U.S. healthcare system as a whole. If we can begin to get a better handle on the ever-growing costs associated with treating chronic health conditions, our healthcare system can then turn more of its attention to prevention. Industry leaders are fully aware that one of the most effective ways to drive down healthcare costs and improve patient wellbeing is through effective prevention, but it's hard to focus on this when so many Americans are already in the grip of chronic disease. With RPM, access to care is greatly expanded and changes in health status can be addressed quickly to avoid crisis and costly hospital admissions and readmissions. Such reduction in urgent and emergent care would translate to substantial annual savings.
The U.S. healthcare system will also benefit from remote patient monitoring by allowing more patients to be cared for even in the face of the looming practitioner shortage. With fewer in-office visits for patients with chronic health conditions, there will be more capacity for other types of office visits, more specifically those that could not be supported virtually. Practitioners will also have the benefit of support from their team to help keep tabs on their patients enrolled in RPM, thus removing some care burdens from practitioners themselves.
The Future of Remote Patient Monitoring
Remote patient monitoring has been quietly evolving for decades. Thanks, in part, to the pandemic and rapid acceptance and adoption of telehealth and telemedicine services, RPM has become a more integral part of our healthcare delivery system. Medicare and private health insurers are taking note of the cost-effectiveness and positive health outcomes associated with RPM, resulting in better access to the service for those patients who benefit most from RPM. Moving forward, patient and practitioner understanding of RPM will continue to rise and technology will become more sophisticated, which should spur further adoption and usage.
Furthermore, remote patient monitoring can help keep vulnerable patients healthy while still allowing practitioners to monitor chronic health conditions closely and effectively. RPM promises to help further drive down individual and overall costs of healthcare through more effective management of care while avoiding expenses associated with emergencies and admissions. With all these very real benefits of remote patient monitoring, it's likely only a matter of time until RPM becomes a standard service for most practices.
If you are interested in taking a deeper dive into remote patient monitoring and how developing an RPM program can benefit your healthcare organization and patients, we encourage you to download this comprehensive guide.