Over just the past few years, the usage and application of telehealth services have begun to grow tremendously, fueled largely by the pandemic.
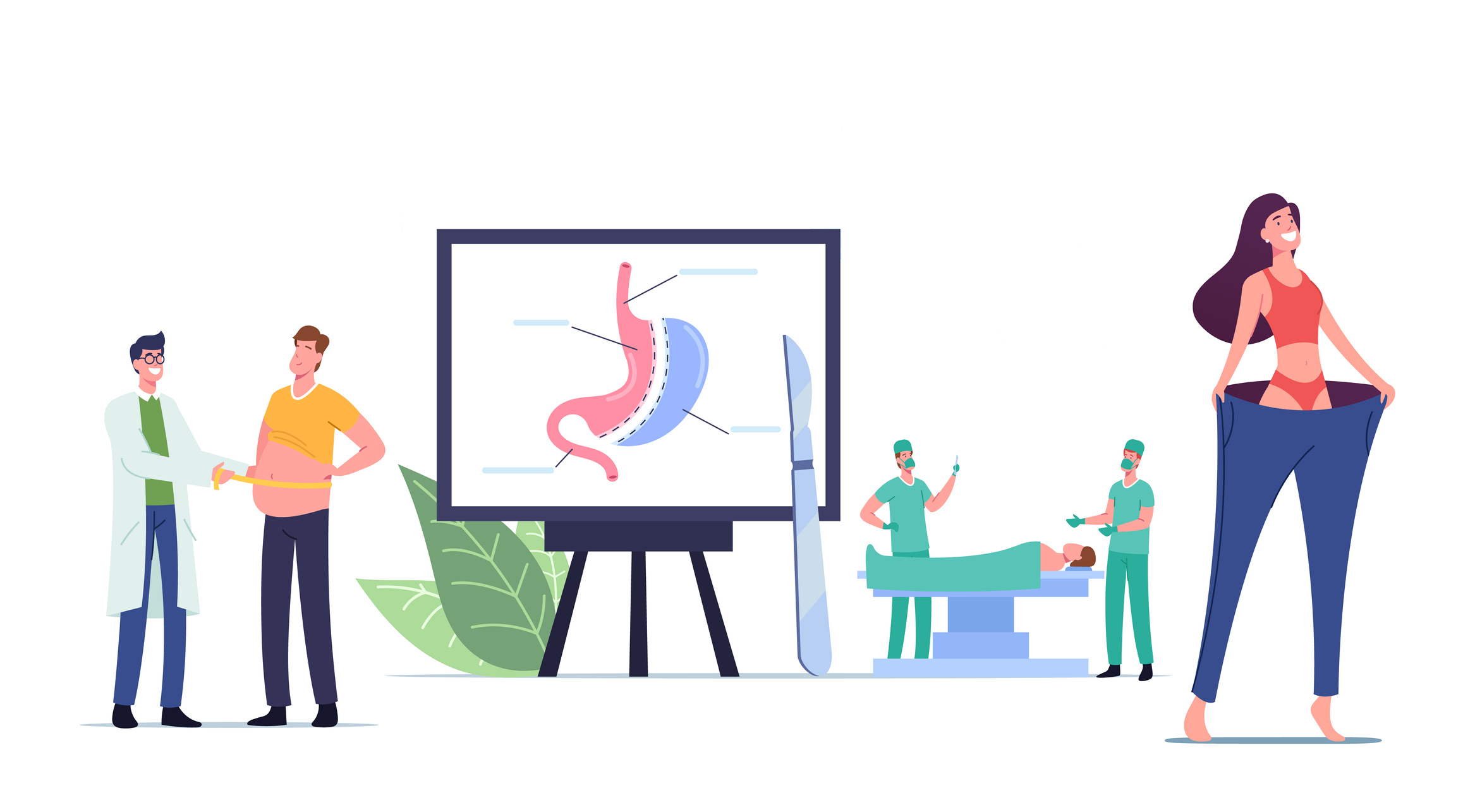
As a result, the world of healthcare is becoming increasingly digitally connected to patients, and technology is serving new and exciting purposes throughout the entire healthcare paradigm. Specific telehealth services, such as remote patient monitoring (RPM), are solidifying a permanent foothold in the care delivered to chronic care management patients due to their ease of use its ability to increase practice efficiency while remaining cost-effective. But could it be argued that RPM may have practical applications in other areas of care, such as bariatric surgery?
The most common benefits of remote patient monitoring could certainly be applied to the bariatric surgery process. Ease of use, convenience, efficiency, and cost-effectiveness are all positive attributes of RPM that benefit its overall application and would lend themselves well to the bariatric surgery specialty. One could even argue that the use of remote patient monitoring may help bariatric surgery patients be more successful in reaching their long-term goals while providing evidential documentation to fulfill payer requirements throughout the phases of the bariatric surgery process, preoperatively to postoperatively, and even beyond.
Benefits of Remote Patient Monitoring Before Bariatric Surgery
The number of patients seeking surgical weight loss solutions is growing. At least 256,000 people underwent some form of bariatric surgical procedure in 2019, according to the American Society for Metabolic and Bariatric Surgery (AMBS). And yet we know from studies that a significant percentage of patients eligible and scheduled for bariatric surgery will not receive the surgical intervention. The most common reasons for cancellation tend to concern patient-related issues, such as patients gaining weight during the preoperative evaluation period. This is often the result of a failure to make appropriate changes to eating and/or exercise habits.
Bariatric surgical candidates are typically required to lower their daily calorie intake to a range determined by the performing surgeon. Using RPM, bariatric surgeons can closely monitor the weight of their surgical candidates and act promptly when weight changes — or lack thereof — jeopardize the likelihood of the procedure proceeding as planned. Such actions can include recommending additional presurgical lifestyle classes, modifications to the personalized lifestyle preparation and diet, and additional guidance and solutions to help patients meet preoperative requirements.
In addition, because of its popularity and associated expense, most patients with insurance seeking bariatric surgery will encounter a lengthy list of qualifying criteria and obstacles to maneuver to meet payer requirements. Insurance-related issues are another common reason why bariatric surgery is cancelled.
The good news is that remote patient monitoring might just be the missing puzzle piece that can help bring the process together, streamlining the approval process and providing supporting evidence to meet documentation requirements. Using RPM digitally connected technology, like smart weight scales, may motivate patients to stay on track and enable their healthcare team to find the best way to support those who are just beginning their bariatric surgery weight loss journey.
Between best practice guidelines set forth by the AMBS and the myriad barriers often put forth by payers, getting approval to undergo bariatric surgery can be challenging for even the most qualified patients. Medicare, which often sets the bar for other payers, requires that the following guidelines be met prior to a Medicare beneficiary undergoing Medicare-covered bariatric surgery:
- Body mass index (BMI) of 35 or greater
- At least one co-morbidity
- Documentation that evidences the patient has been obese for the last 5 years
- Documentation that evidences participation in a medically supervised weight loss programs (tried and failed more than one program)
- A letter from the primary care provider in support of weight loss surgery
- Patient must pass a psychological evaluation
- Documentation that all other possible treatable medical causes or disease have been ruled out as the possible cause of the patient's obesity
It usually takes several months for a patient to meet all the aforementioned qualifying preoperative and insurance conditions to proceed with a bariatric surgical procedure. To help patients stay on a reasonable timeline, remote patient monitoring may lend some convenient support to the pre-surgery qualification process, especially concerning the documentation required that provides evidence of the patient's failed attempts in supervised weight loss programs. Prior to bariatric surgery, previous use of RPM may also help provide evidence of the patient's history with obesity and help solidify proof and severity of other co-morbidities, such as diabetes, hypertension, or asthma. With an array of different remote patient monitoring devices that can track the symptoms and associated exacerbations of several different chronic diseases, RPM can supply practitioners with the necessary evidence to proceed with surgery and receive reimbursement.
Importance of Remote Patient Monitoring for Medically Supervised Weight Loss Programs
Patients pursuing bariatric surgery for weight loss will need to follow a medically supervised weight loss program to qualify for insurance coverage. Ultimately, the goal of these programs is to ensure the patient is committed to the program requirements both preoperatively and postoperatively and to help their body prepare for the invasive procedure.
For insurance coverage, most medically supervised weight loss programs are required to last 3–6 months. They are aimed at educating the patient and ensuring the patient is willing and able to commit to the long-term end goal. While participation in weight loss programs is required for payer approval, the patient doesn't necessarily need to be successful in losing weight, hence the "tried-and-failed" requirement. Remote patient monitoring is a valuable tool in tracking the patient's willingness to participate in a medically supervised weight loss program on top of its general, valuable applications.
Value of Remote Patient Monitoring Following Bariatric Surgery
According to ASMBS, more than 95% of patients will successfully lose at least half of their extra body weight immediately following surgery. Many people lose an average of 20% of their excess weight by two months following surgery. Weight loss happens quickly, and in a perfect world, it would continue unhindered until the patient met their goal.
However, this is not always the case. Adherence to lifestyle habits and changes that must be adjusted after bariatric surgery can prove difficult for some patients, leading them to lose weight at a slower pace or even regaining weight.
Since many patients need wraparound support following bariatric surgery, the postoperative and follow-up care schedule is both important and intensive. For most, visits with their weight loss management team will occur fairly frequently immediately following surgery, with visits occurring every three months at a minimum for the first year. During the second year, most participants follow up with their team every 6–12 months, with ongoing annual visits indefinitely. During the early postoperative period, remote patient monitoring can be utilized as a convenient tool for tracking a patient's weight management success and help prevent or stop backslides in weight gain before it can become a more significant problem.
Using Remote Patient Monitoring to Help Patients Stay on Track
Over the long term, remote patient monitoring can prove useful to patients as they navigate their new way of life in the years following their bariatric surgical procedure. With less frequent physical check-ins with their healthcare team, patients sometimes begin to revert to old habits and can unwittingly undo hard-earned weight loss. As noted by Healthline, the excess weight loss for most bariatric surgery patients decreased to 56% just five years after their procedure, making overall, long-term results frustratingly small.
While payer support of remote patient monitoring past the improvement of chronic health conditions is uncommon, that will hopefully change. Occasional periods of RPM for bariatric patients, especially when a patient is struggling with maintaining or losing weight, can contribute to increased accountability and engagement, helping patients remain successful in keeping weight off in the years well beyond their bariatric surgical procedure.
The Case for Bariatric Surgery Remote Patient Monitoring
Bariatric surgery can lead to life-changing outcomes for obese patients, decreasing or even eliminating co-morbidities and allowing them to live longer, more active lives. Prior to surgery, remote patient monitoring can help patients and practitioners meet the myriad preoperative requirements. Immediately following a bariatric surgical procedure and even in the years beyond, RPM can help patients stay on track and keep them better connected to their healthcare team. With the rise of obesity-related chronic health conditions, intertwining remote patient monitoring throughout the entire gastric surgery process could help combat cost, increase surgical effectiveness, and create efficiencies for patients, payers, and practitioners alike.